[HGPI Policy Column] No. 33 – From the NCDs (Precision Cancer Medicine) Team, What is precision cancer medicine?
date : 2/2/2023
![[HGPI Policy Column] No. 33 – From the NCDs (Precision Cancer Medicine) Team, What is precision cancer medicine?](https://hgpi.org/en/wp-content/uploads/sites/2/column-33-top.png)
1. In treating cancer, there are three major therapies, namely, (i) Surgical operation, (ii) Radiation therapy, and (iii) Drug therapy (Chemotherapy). Recently, treatment options have been increasing—for example, (iv) Cancer immunotherapy, which uses treatments to stimulate or restore the ability of the immune system to fight cancer, has become one of the major treatment options (see table below).
“Precision cancer medicine,” which has been attracting attention in recent years, is particularly related to (iii) Drug therapy. They identify the mutated genes, cancer cells of individual patients to be treated in advance, and then, “molecular-targeted drugs” (drugs that are particularly effective on those mutated genes and molecules) are selected and administered.
In conventional cancer drug therapy, cancers are usually perceived in terms of the affected organ, and drugs are administered with the expectation they will be effective for that type of cancer. In precision cancer medicine, they provide treatment in a more targeted manner, by focusing on the section of the gene where mutations are occurring. This is why it is called “precision” medicine.
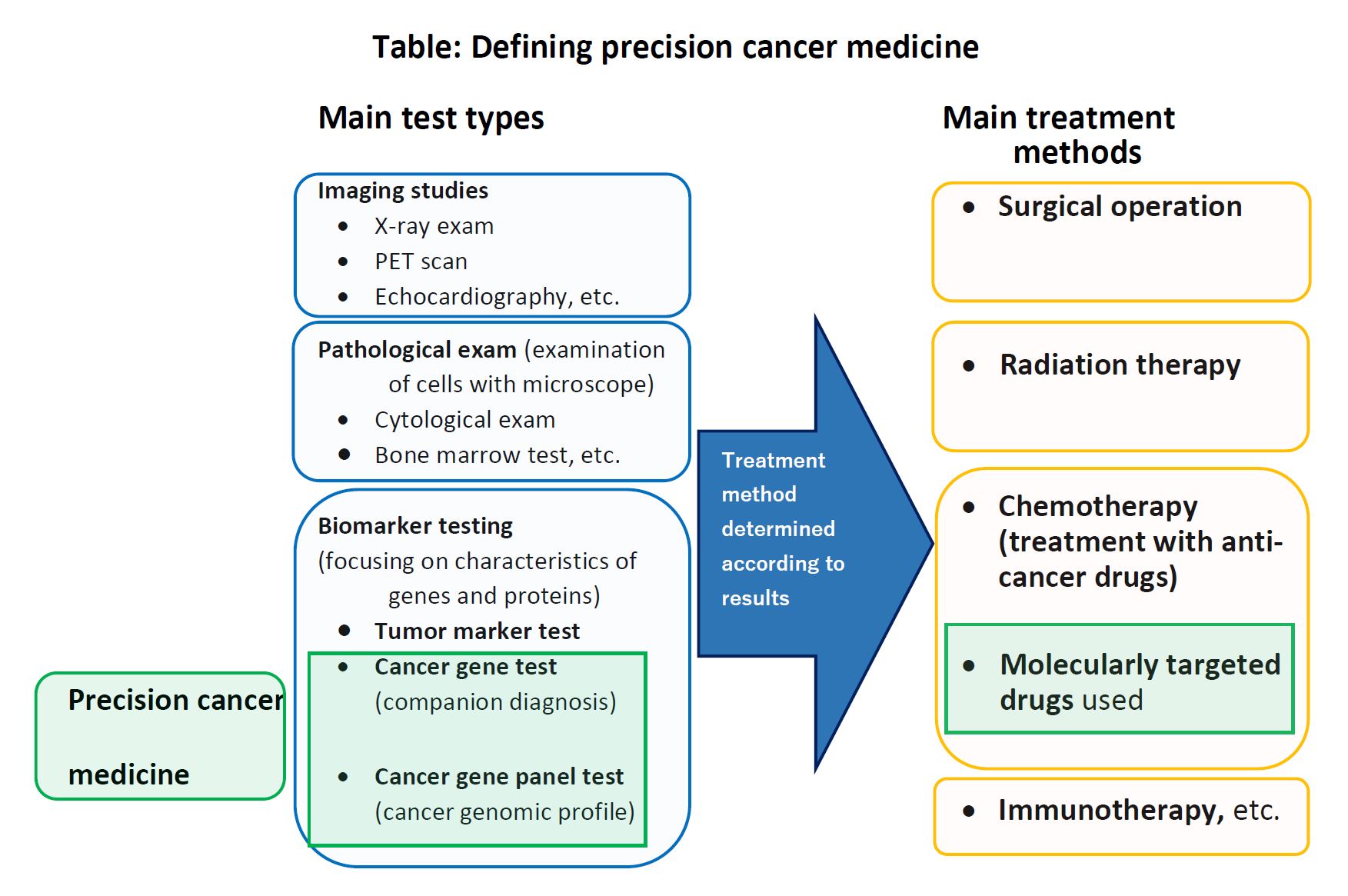
2. To carry out precision cancer medicine, genetic testing is indispensable. There are two methods of genetic testing for cancer: (i) “Cancer gene testing “or “Companion diagnostic testing” and (ii) “Cancer gene panel testing” or “Cancer genome profiling test.” Cancer gene testing determines the presence or absence of mutations in one or several genes, in order to determine in advance whether a certain therapeutic drug will be effective for a patient’s cancer. Cancer gene panel testing is to determine the presence or absence of mutations in a large number of genes (usually more than one hundred) at once.
3. Compared to conventional cancer drug therapy, more targeted therapies are administered in precision cancer medicine, and this can reduce burdens on patients, increase response rates, and achieve better outcomes. There are high expectations for the future development of precision cancer medicine.
On the other hand, there are many challenges: (a) the costs of testing and treatment are often quite expensive; (b) even if a genetic testing is conducted, it may not find a genetic mutation that is eligible for precision cancer medicine (in such a case, conventional drug therapy is an option); (c) nationwide, specialized facilities and human resources to conduct genetic testing and treatment are not that abundant; and (d) laws and regulations to strictly manage genetic information and to prevent genetic discrimination have not yet been fully established.
In order to further develop precision cancer medicine in the future, it is necessary to resolve these various issues as soon as possible.
Column authors
- Sayaka Honda (Program Specialist, HGPI)
- Osamu Takemoto (Program Specialist, HGPI)
- Haruka Sakamoto (Senior Manager, HGPI)
HGPI Policy Column (No.32) -From thePlanetary Health Policy Team- >
日本語
Top Research & Recommendations Posts
- [Announcement] HGPI Joins Alliance for Transformative Action on Climate and Health (April 22, 2024)
- [Announcement] A Significant Step Towards the Building a Green Healthcare System: Support for the Formal Expression of Interest by the Japanese Government Delegation to the ATACH at the Executive Board Meeting of the WHO (February 16, 2024)
- [Research Report] Building a Mental Health Program for Children and Measuring its Effectiveness (June 16, 2022)
- [Research Report] Survey of Japanese Physicians Regarding Climate Change and Health (December 3, 2023)
- [Research Report] 2019 Survey on Healthcare in Japan
- [Policy Recommendations] Obesity Control Promotion Project 2023 “The Next Steps for Engaging and Cooperating with Patients, Citizens, and Communities for Implements of Obesity Control Measurements” (April 8, 2024)
- [Event Report] Planetary Health Expert Meeting Aiming for Sustainable Healthcare: Learning from the Impact of Environmental Pollution and Medical Waste During the Pandemic (February 16, 2024)
- [Publication Report] Developing and Expanding Cardiovascular Disease Control Plans in Each Prefecture – Challenges and Good Examples for Cardiovascular Disease Control (September 7, 2023)
- [Report and Recommendations] Discussion Points in Healthcare DX Project Expert Panel Meeting (April 2, 2024)
- [Announcement] HGPI Joins Global Climate and Health Alliance (March 23, 2024)
Featured Posts
-
2024-04-22
[Registration Open] (Hybrid Format) Intractable Disease Day Symposium: Future Measures for Intractable Diseases from the Perspectives of Patients and Citizens (May, 23 2024)
![[Registration Open] (Hybrid Format) Intractable Disease Day Symposium: Future Measures for Intractable Diseases from the Perspectives of Patients and Citizens (May, 23 2024)](https://hgpi.org/en/wp-content/uploads/sites/2/236ac5baafb5dca3088d99dc7210efc1.jpg)
-
2024-04-23
[Registration Open] (Webinar) The 125th HGPI Seminar: Progress and Prospects for Domestic Measures on Health Problems Caused by Alcohol (May 24 , 2024)
![[Registration Open] (Webinar) The 125th HGPI Seminar: Progress and Prospects for Domestic Measures on Health Problems Caused by Alcohol (May 24 , 2024)](https://hgpi.org/en/wp-content/uploads/sites/2/HGPI_20240524_125thHGPIseminar_Eyecatch_rev.jpg)
-
2024-04-30
[Event Report] Non-partisan Diet Member Briefing – 30-minute Health Policy Update: “Community Development for Senior Health: From Establishing Evidence to Social Implementation” (April 23, 2024)
![[Event Report] Non-partisan Diet Member Briefing – 30-minute Health Policy Update: “Community Development for Senior Health: From Establishing Evidence to Social Implementation” (April 23, 2024)](https://hgpi.org/en/wp-content/uploads/sites/2/cb69d3b6d57341513e48578b7133bdb6-scaled-1.jpg)
-
2024-05-02
[Event Report] The 123rd HGPI Seminar – The Current Situation and Future Prospects for Epilepsy in Japan and Around the World (March 6, 2024)
![[Event Report] The 123rd HGPI Seminar – The Current Situation and Future Prospects for Epilepsy in Japan and Around the World (March 6, 2024)](https://hgpi.org/en/wp-content/uploads/sites/2/hs123-top-20th_ver.02-1.png)
-
2024-05-09
[Registration Open] The Health Policy Academy the 13th Session
![[Registration Open] The Health Policy Academy the 13th Session](https://hgpi.org/en/wp-content/uploads/sites/2/HGPI_20240508_HPA13th_registration.png)




